Double Vision from Strabismus: Vision Therapy Guide
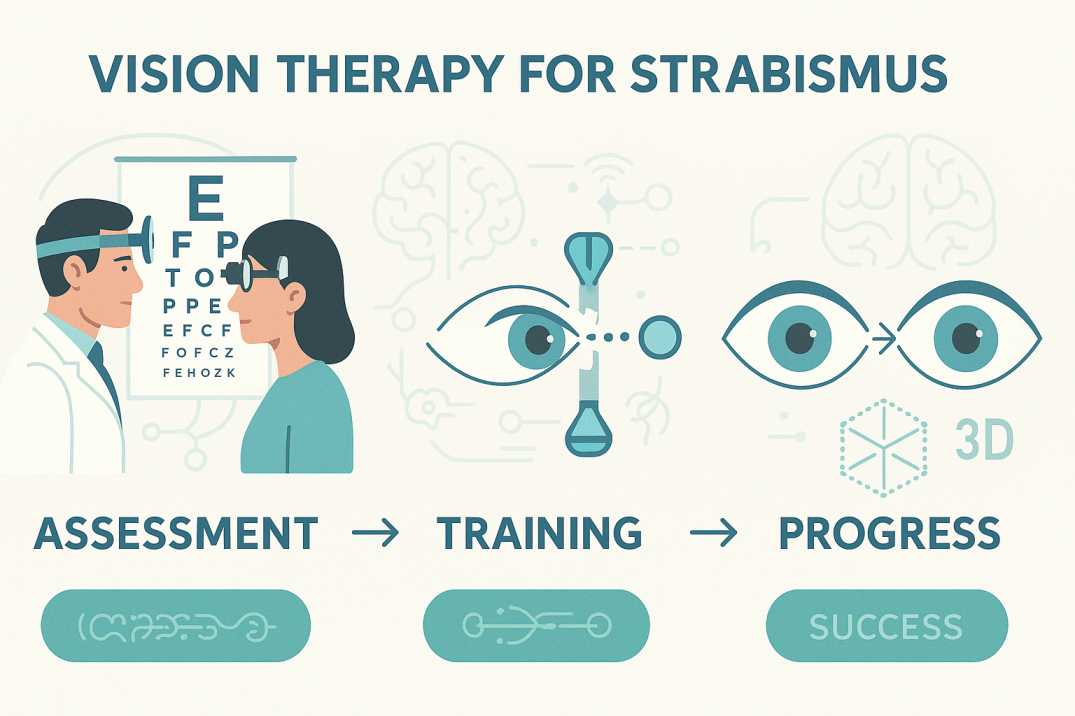
Executive Summary: Vision therapy offers proven double vision treatment for strabismus patients, with success rates of 75-87% in achieving both functional binocular vision and cosmetic alignment. Unlike surgery that only addresses cosmetic appearance, vision therapy retrains the brain-eye connection to provide lasting improvements in eye coordination, depth perception, and quality of life.
When your eyes fail to work together as a coordinated team, the world transforms into a confusing and overwhelming visual experience. Double vision from strabismus affects millions of people globally, turning routine daily activities—reading, driving, or navigating stairs—into significant challenges. However, modern vision therapy offers evidence-based hope for lasting improvement through proven eye exercises for strabismus treatment, eliminating the risks and limitations associated with surgical intervention.
What Causes Double Vision in Strabismus Patients?
Double vision (diplopia) from strabismus occurs when misaligned eyes transmit conflicting images to the brain. Unlike refractive errors that can be corrected with glasses alone, this condition stems from a neurological coordination dysfunction between the brain and extraocular muscles.
Recent comprehensive studies show strabismus affects 1.93% of the global population (95% CI: 1.64-2.21), with U.S. prevalence ranging from 2-5% in the general population. The condition commonly presents with double vision, monocular suppression (closing or covering one eye when focusing on nearby objects), and compensatory head positioning.
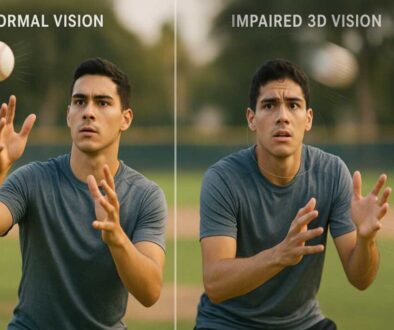
This condition extends far beyond cosmetic concerns, significantly impacting depth perception, reading comprehension, and overall quality of life. The neurological complexity requires sophisticated treatment approaches that address the underlying brain-eye coordination deficits.
Understanding the Neurological Mechanism
When strabismus develops in adulthood, the brain cannot simply suppress input from one eye, and double vision emerges as a debilitating symptom. The brain simultaneously receives two disparate images—one from each eye—creating characteristic double vision patterns:
- Horizontal diplopia: Images appear laterally displaced
- Vertical diplopia: Images appear vertically separated
- Diagonal diplopia: Images appear angularly displaced
- Intermittent diplopia: Double vision that occurs episodically
The Neuroscience Behind Vision Therapy for Strabismus
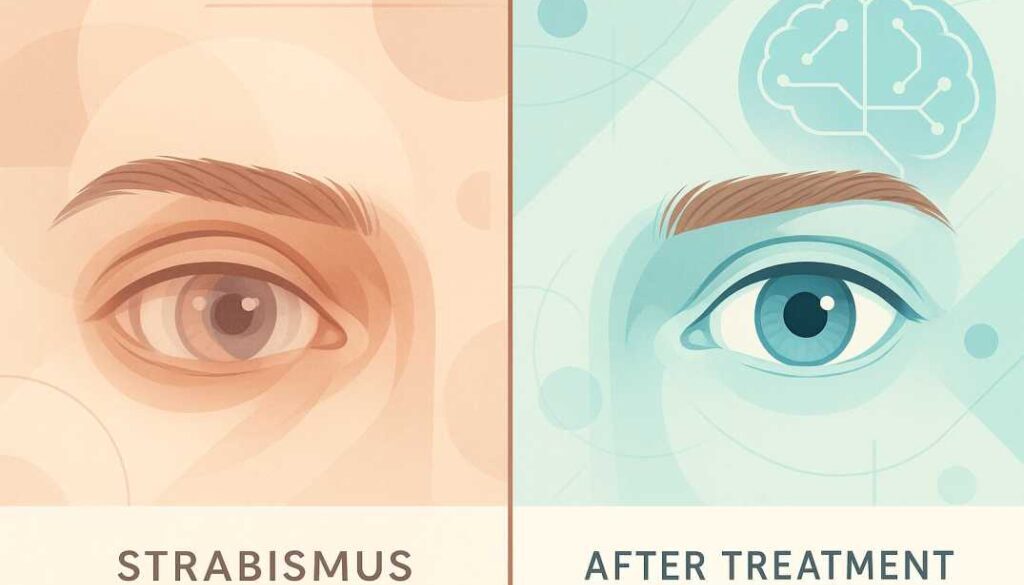
Vision therapy addresses the neurological root cause rather than merely treating symptoms. This evidence-based approach utilizes doctor-supervised, in-office exercises that effectively train the eyes, brain, and body to eliminate or significantly reduce double vision. The exercises modify brain function at the neurological control center that governs extraocular muscle coordination.
Three Essential Principles of Effective Strabismus Treatment
Contemporary strabismus treatment through vision therapy focuses on three fundamental principles: equalizing individual eye function, developing central-peripheral vision integration, and establishing coordinated binocular function.
1. Equalizing Eye Function Each eye must demonstrate comparable efficiency in saccadic movements, accommodative function, and visual processing capabilities.
2. Central-Peripheral Integration: Achieving optimal balance between detailed foveal vision and spatial peripheral awareness for comprehensive visual processing.
3. Binocular Coordination Training both eyes to fixate simultaneously on identical spatial locations with proper vergence control.
Neuroplasticity: The Foundation for Adult Treatment
Recent research has revolutionized our understanding of adult neurological adaptability. Adults with long-standing, constant strabismus can achieve random dot stereopsis through optometric vision therapy, demonstrating that neuroplasticity extends significantly beyond childhood critical periods.
The neuroplasticity principle ensures that therapeutic results are enduring and achievable at any age. Contemporary understanding confirms that it is never too late to eliminate double vision and develop superior binocular vision through systematic vision therapy.
Evidence-Based Success Rates: Vision Therapy vs. Surgical Intervention
Vision Therapy Clinical Outcomes
Peer-reviewed research demonstrates that vision therapy achieves success rates of 75-87% in establishing both functional binocular vision and cosmetic alignment in strabismus patients. Studies specifically show up to 88% effectiveness for convergence insufficiency and related binocular anomalies.
Surgical Limitations and Realistic Expectations
While surgical success rates are often quoted at 60-80%, these statistics primarily measure cosmetic improvement rather than functional visual enhancement. Comprehensive studies of infantile esotropia demonstrate surgical success rates of only 22% for achieving functional binocular vision, while a 1987 study of acquired esotropia showed merely 15% functional success in 1,170 patients.
Surgery frequently achieves cosmetic eye straightening but fails to address visual sensory perception and binocular fusion, which can contribute to post-operative diplopia development.
Eye Exercises for Strabismus: Professional Vision Therapy Techniques
Core Eye Exercises for Strabismus Treatment
1. Pencil Push-ups (Convergence Training) Patients hold a pencil at arm’s length, focus on the tip, and gradually move it toward the nose while maintaining single vision. When diplopia occurs, patients pause and refocus until the image becomes singular.
2. Brock String Exercise
Utilizing a 5-foot string with three colored beads, patients focus on each bead while observing the correct “X” pattern formation, indicating proper binocular fusion and vergence control.
3. Computer-Based Vision Therapy: Interactive software programs designed to enhance eye tracking, accommodative function, and binocular coordination, often incorporating virtual reality and therapeutic gaming elements to address depth perception deficits.
4. Prism Adaptation Training: Specialized therapeutic lenses that facilitate binocular coordination training, with gradual prism reduction as binocular function improves.
Professional Supervision vs. Home-Based Programs
While basic exercises can provide limited benefit, professional vision therapy conducted by certified practitioners over structured treatment periods using a combination of in-office and home-based protocols demonstrates significantly superior outcomes compared to unsupervised eye exercises.
Patient Demographics: Treatment Efficacy Across Age Groups
Pediatric Patients: Neuroplasticity Advantage
Children’s developing visual systems demonstrate exceptional responsiveness to vision therapy. Early intervention remains crucial, as younger patients often achieve more rapid treatment responses due to enhanced brain adaptability and increased neuroplasticity for visual pathway retraining.
Adult Patients: Challenging the “Critical Period” Myth
Contemporary research demonstrates that adults can achieve significant improvements through dedicated therapy protocols. While treatment duration may extend longer than pediatric cases, adults can achieve meaningful improvements in eye alignment, diplopia reduction, and enhanced quality of life.
Case studies document adults with unilateral small-angle esotropia achieving random dot stereopsis following optometric vision therapy, with one 33-year-old patient successfully achieving virtual reality perception and 20/25 visual acuity.
Double Vision Treatment Cost: Vision Therapy vs. Surgery
Treatment Timeline and Investment Analysis
Typical Treatment Parameters:
- Assessment Phase: 1-2 comprehensive functional evaluations
- Active Treatment: 3-9 months of weekly supervised sessions
- Maintenance Phase: Gradual session reduction with home exercise protocols
- Total Program Duration: 6-12 months for optimal outcomes
Early Progress Indicators
Many patients demonstrate noticeable improvements within 2-4 weeks, with documented cases reporting complete book reading capability without visual interruption for the first time following just two weeks of tracking exercises.
Financial Investment Comparison
Vision therapy programs typically cost $2,800-$4,000 total, with individual sessions ranging from $125-$250, compared to strabismus surgery costs of $5,000-$10,000. The cost-effectiveness ratio strongly favors vision therapy when considering functional outcomes rather than purely cosmetic results.
Recent Scientific Validation: 2024-2025 Research Findings
Study 1: Enhanced Amblyopia Treatment Integration
A 2024 randomized trial published in Ophthalmic and Physiological Optics demonstrated that active vision therapy combined with occlusion therapy showed superior results compared to occlusion alone, with significant improvements in visual acuity and binocular function metrics.
Study 2: Long-term Pediatric Efficacy
A comprehensive 2022 study documented the long-term efficacy of combined occlusion and active vision therapy in 27 amblyopic children, demonstrating sustained improvements in both distance and near visual acuity as well as binocular function lasting up to two years post-treatment completion.
Study 3: Adult Neuroplasticity Breakthrough
A 2024 case series published in Clinical Insights in Eyecare documented three adults with unilateral small-angle esotropia who achieved random dot stereopsis following optometric vision therapy, fundamentally challenging previous assumptions regarding adult treatment limitations.
Treatment Selection Criteria and Clinical Decision-Making
Optimal Vision Therapy Candidates
Vision therapy demonstrates maximum effectiveness for patients presenting with:
- Intermittent strabismus with variable manifestation patterns
- Small to moderate eye deviations (under 25-30 prism diopters)
- Adequate visual acuity in both eyes
- Strong patient motivation for treatment compliance
- Absence of significant structural ocular pathology
Integrated Treatment Protocols
The evidence-based treatment algorithm includes optical correction, pharmaceutical interventions when indicated, binocular vision therapy, and surgical consultation when necessary, with vision therapy both preceding and following surgical intervention for optimal functional outcomes.
Daily Life Management and Long-term Quality Improvements
Immediate Coping Strategies
During vision therapy treatment progression:
- Optimal lighting conditions to minimize visual strain
- Regular visual rest intervals during sustained near tasks
- Proper ergonomic positioning of reading materials and visual displays
- Consideration of temporary prism correction for severe diplopia cases
- Maintenance of proper posture to support optimal visual alignment
Long-term Functional Improvements
Success case studies consistently document transformative outcomes: children who previously could not participate in sports activities achieving athletic success, adults regaining driving confidence and vocational performance, and families experiencing relief from years of educational and developmental challenges.
Making Evidence-Based Treatment Decisions
Clinical Indicators for Vision Therapy Success
Vision therapy demonstrates optimal effectiveness for patients presenting with intermittent strabismus manifestations, small to moderate eye deviations, adequate bilateral visual acuity, strong treatment motivation, and absence of significant structural ocular pathology.
Integrated Treatment Approaches
Contemporary evidence-based protocols incorporate optical correction, pharmaceutical interventions when indicated, comprehensive binocular vision therapy, and surgical consultation when necessary, with vision therapy providing both pre- and post-surgical support for optimal functional outcomes.
References and Resources
Key Scientific Studies Supporting Vision Therapy for Strabismus
-
Hashemi, H., Pakzad, R., Heydarian, S., et al. (2019). “Global and regional prevalence of strabismus: a comprehensive systematic review and meta-analysis.” Strabismus, 27(2), 54-65.
https://pubmed.ncbi.nlm.nih.gov/31012389/
This comprehensive meta-analysis of 56 studies with 229,396 participants established the current global prevalence of strabismus at 1.93% and provides the foundation for understanding the scope of this condition worldwide. -
Han, S., Baker, J., & Jenewein, E. (2024). “Case Series: Neuroplasticity and Vision Therapy in Adults with Unilateral Small-Angle Esotropia.” Clinical Insights in Eyecare, 2(2).
https://clinicalinsightsineyecare.scholasticahq.com/article/94928-case-series-neuroplasticity-and-vision-therapy-in-adults-with-unilateral-small-angle-esotropia
This 2024 case series demonstrates that adults with long-standing constant strabismus can achieve random dot stereopsis after optometric vision therapy, challenging previous assumptions about adult treatment limitations. -
Piñero, D.P., Gil-Casas, A., Hurtado-Ceña, F.J., & Molina-Martin, A. (2022). “Long-Term Efficacy of the Combination of Active Vision Therapy and Occlusion in Children with Strabismic and Anisometropic Amblyopia.” Children, 9(7), 1007.
https://pubmed.ncbi.nlm.nih.gov/35883996/
This retrospective study evaluated 27 amblyopic children over two years, showing significant improvements in both distance and near visual acuity and binocular function, with sustained results lasting up to two years post-treatment.
Conclusion: The Path to Visual Transformation
Evidence-based vision therapy offers superior functional outcomes for strabismus patients seeking double vision treatment. With documented success rates of 75-87% for achieving both cosmetic alignment and binocular vision function, vision therapy addresses neurological root causes while surgical interventions typically treat only symptoms.
Early intervention optimizes treatment outcomes across all age groups. Pediatric patients benefit from enhanced neuroplasticity, while contemporary research confirms that adults can achieve significant functional improvements that substantially enhance quality of life.
Professional evaluation and treatment planning remain essential for optimal outcomes. Comprehensive functional vision assessment by qualified vision therapy providers ensures accurate diagnosis and personalized treatment protocol development.
The evidence overwhelmingly supports vision therapy as the primary treatment modality for functional double vision resolution, offering patients hope for lasting visual transformation without surgical risks or limitations.
Ready to explore evidence-based treatment options? Learn more about vision therapy for children
About Cook Vision Therapy Center
With over four decades of specialized clinical experience, Dr. David Cook has successfully treated thousands of patients for strabismus and double vision using evidence-based, non-surgical protocols. Located in Marietta, Georgia, Cook Vision Therapy Center provides comprehensive functional vision evaluations and personalized treatment programs designed to address individual visual system needs.
Ready to begin your visual transformation journey? Contact Cook Vision Therapy Center today to schedule your comprehensive evaluation and take the first step toward clearer, more comfortable binocular vision.
Disclaimer: This article is intended for educational and informational purposes only and should not be construed as medical advice. Always consult with qualified healthcare professionals for diagnosis and treatment recommendations specific to individual circumstances. Vision therapy outcomes may vary based on individual patient factors and treatment compliance.
FAQs
-
Double vision (diplopia) from strabismus occurs when misaligned eyes send conflicting images to the brain, causing overlapping or side-by-side visual distortions.