Vision Therapy Games vs Patching: Best Lazy Eye Treatment 2025
Vision Therapy Games vs. Patching: Which Works Better for Lazy Eye?
A comprehensive evidence-based analysis of modern amblyopia treatment options
When your child receives an amblyopia diagnosis—commonly known as lazy eye—you’re confronted with treatment decisions that can feel overwhelming. Should you pursue traditional patching treatment or explore innovative amblyopia games and digital vision therapy technologies? This comprehensive guide examines the latest peer-reviewed research to help you make an informed, evidence-based decision about the most effective patching treatment vs the amblyopia game approach for your family’s unique situation.
Understanding Amblyopia: Beyond the “Lazy Eye” Misconception
Amblyopia affects approximately 1-5% of children worldwide, representing the most prevalent cause of monocular vision loss in pediatric populations. Despite its colloquial designation as “lazy eye,” this characterization fundamentally misrepresents the condition—amblyopia is a sophisticated neurodevelopmental disorder wherein the brain preferentially processes visual input from one eye over the other, resulting in compromised vision development in the suppressed eye.
The etiology of amblyopia typically involves ocular imbalances arising from:
Primary Risk Factors:
- Strabismus (ocular misalignment or crossed eyes)
- Anisometropia (significant refractive error disparity between eyes)
- Deprivation amblyopia (visual obstruction from cataracts, ptosis, or other anatomical barriers)
Early therapeutic intervention proves critical because the visual system demonstrates peak neuroplasticity during childhood development, with optimal treatment outcomes occurring before the critical period closes around ages 8-9 years. This critical period, known as visual plasticity, determines how effectively lazy eye therapy, occlusion treatment, and binocular vision training can restore normal sight development.
Traditional Patching Treatment: Evidence-Based Foundation
Mechanism of Action and Clinical Protocol
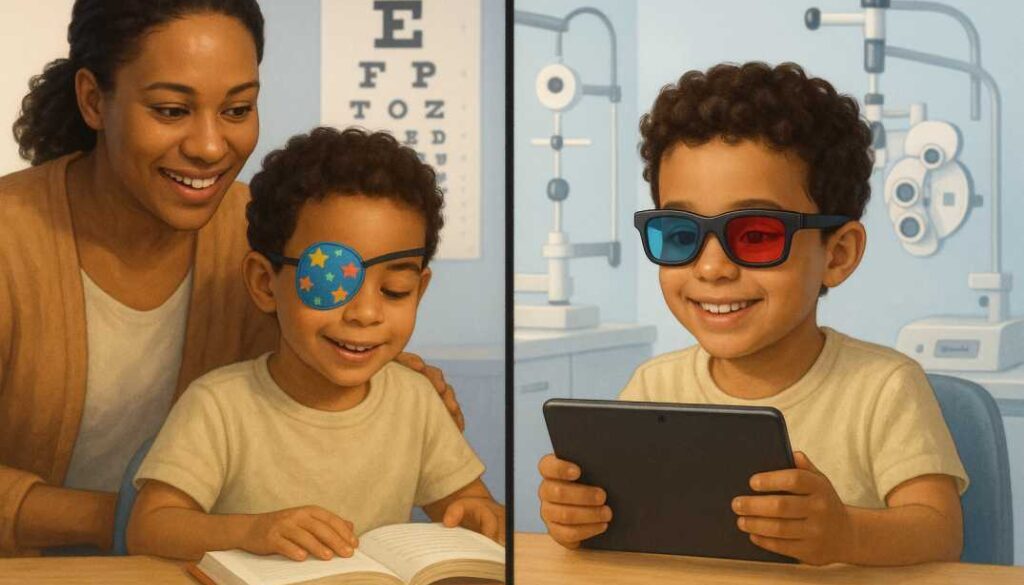
Patching treatment employs occlusion therapy, systematically covering the dominant eye with an adhesive patch for prescribed durations daily, compelling the brain to utilize and strengthen the amblyopic eye. This therapeutic approach has maintained its position as the cornerstone of amblyopia treatment for over two centuries, with substantial evidence supporting its efficacy across diverse patient populations.
The landmark 2024 EuPatch study, published in The Lancet, fundamentally transformed patching protocols through rigorous multicenter analysis. This pivotal research, encompassing 334 children across five European countries, demonstrated that early intensive patching protocols significantly outperform extended optical treatment approaches, challenging traditional clinical guidelines that recommended prolonged spectacle adaptation periods.
Evidence-Based Clinical Outcomes
Treatment Efficacy Metrics:
- Primary endpoint success: 67% of participants achieved treatment success with early patching protocols compared to 54% with extended optical treatment approaches
- Optimal intervention timing: Initiating patching after 3 weeks of refractive correction demonstrates superior efficacy compared to 18-week delays
- Personalized treatment algorithms: Children under 5 years, 4 months with mild amblyopia (≤0.6 logMAR) may benefit from extended optical treatment as first-line therapy
Dosage-Dependent Treatment Response
Contemporary evidence supports stratified patching protocols based on amblyopia severity:
Moderate Amblyopia (20/40 to 20/80):
- 2 hours daily occlusion demonstrates equivalent efficacy to 6-hour protocols
- Treatment response is typically evident within 6-12 weeks
Severe Amblyopia (20/100 to 20/400):
- 6 hours daily occlusion matches full-time patching effectiveness
- Sustained improvement requires 3-6 months of consistent intervention
Treatment Duration: Peak visual improvement occurs within the initial 3-6 months, with maintenance protocols preventing regression in 75% of successfully treated patients.
Digital Vision Therapy: The Paradigm Shift
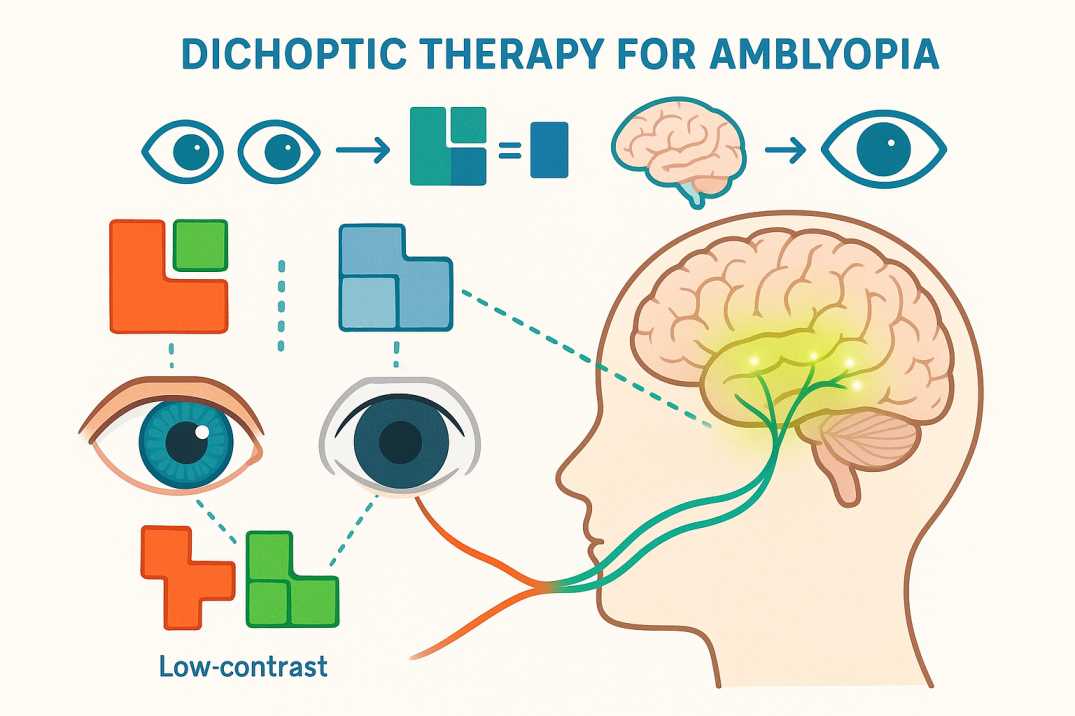
Dichoptic Therapy and Neuroplasticity Mechanisms
Modern amblyopia games leverage dichoptic therapy—an innovative neuroplasticity-based approach presenting differential visual stimuli to each eye simultaneously. Unlike traditional occlusion therapy, which temporarily suppresses the dominant eye, these digital vision exercises, therapeutic eye games, and computer-based vision training promote active binocular cooperation while selectively training the amblyopic eye through contrast manipulation and depth perception exercises.
Leading Clinical Platforms:
Evidence-Based Solutions:
- AmblyoPlay: Over 25,000 global users with documented treatment outcomes
- CureSight: FDA-cleared eye-tracking system with published non-inferiority data
- Luminopia: VR-based dichoptic therapy with pediatric content libraries
Therapeutic Protocol and Neuroscience Foundation
Dichoptic Training Methodology:
- Binocular image separation: Specialized viewing systems deliver distinct visual information to each eye through anaglyph glasses or VR displays
- Contrast threshold manipulation: The dominant eye receives reduced-contrast stimuli while the amblyopic eye processes high-contrast targets
- Active binocular engagement: Therapeutic games require bilateral eye cooperation for task completion, promoting cortical binocular fusion
- Neuroplasticity optimization: Systematic practice strengthens synaptic connections between the visual cortex and amblyopic eye neural pathways
Comparative Clinical Evidence
Systematic review and meta-analysis of digital therapy effectiveness reveals compelling advantages over traditional approaches:
Enhanced Treatment Compliance:
- Improved therapeutic adherence through gamification psychology
- Documented success in populations with patching treatment failure
- An extended therapeutic window for adult and adolescent patients
- Superior binocular function outcomes compared to monocular training
Accelerated Visual Recovery:
- Some clinical trials demonstrate measurable improvement within 2-4 weeks
- Reduced total treatment duration compared to traditional patching treatment
- Sustained visual gains with lower regression rates
- Enhanced stereoacuity development through binocular stimulation
Comparative Treatment Analysis: Evidence-Based Outcomes
Visual Acuity Improvement: Head-to-Head Clinical Data
Pivotal CureSight Trial (2024) – 149 pediatric participants in a multicenter randomized controlled trial:
Primary Outcome Measures:
- CureSight binocular therapy: 0.28 ± 0.13 logMAR improvement
- Traditional patching protocol: 0.23 ± 0.14 logMAR improvement
- Non-inferiority margin achieved with statistical significance (p<0.0001)
- Individual treatment response demonstrates considerable inter-patient variability
Secondary Endpoints:
- Stereoacuity enhancement is comparable between modalities
- Binocular visual acuity improvement favors the dichoptic approach
- Sustained treatment effects at 12-month follow-up evaluation
Treatment Adherence and Patient Experience
Traditional Patching Limitations:
- Psychosocial challenges, including appearance-related anxiety and peer stigmatization
- Mechanical compliance difficulties with patch removal behaviors
- Limited therapeutic efficacy in adolescent and adult populations
- Potential for occlusion amblyopia development with excessive patching duration
Digital Therapy Advantages:
- 93% parental satisfaction rates with CureSight binocular treatment protocols
- 91% preference for digital therapy over traditional patching treatment for future interventions
- Superior adherence metrics in older pediatric populations (93% vs 78% compliance)
- Seamless integration into contemporary digital lifestyle patterns
Stereoacuity and Binocular Function Outcomes
Contemporary clinical evidence demonstrates equivalent stereoacuity improvement between treatment modalities, with both approaches effectively enhancing three-dimensional visual perception when combined with appropriate strabismus management protocols. Digital therapies may provide additional advantages in binocular function development through active cooperation training rather than monocular suppression techniques.
Evidence-Based Treatment Protocols by Patient Demographics
Pediatric Populations (Ages 3-7): Critical Period Interventions
Optimal Treatment Window Characteristics:
- Maximum neuroplasticity with rapid treatment response potential
- Primary recommendation: Early intensive patching treatment (2-6 hours daily, severity-dependent)
- Adjunctive therapy: Structured near-vision activities during occlusion periods
- Expected timeline: Measurable improvement within 12-16 weeks of consistent intervention
Clinical Rationale: The critical period for visual development necessitates aggressive intervention to maximize neuroplastic potential before cortical maturation limits treatment responsiveness.
School-Age Children (Ages 8-12): Extended Plasticity Management
Treatment Approach for Older Pediatric Patients:
- Evidence-based protocol: Combination therapy utilizing both occlusion and binocular training
- Strategic emphasis: Dichoptic amblyopia games for enhanced engagement and compliance
- Realistic expectations: Gradual but clinically significant improvement over 6-9 months
Scientific Foundation: Recent neuroplasticity research demonstrates continued visual cortex adaptability beyond traditional critical periods, supporting extended treatment protocols for older children.
Adolescent and Adult Populations: Neuroplasticity-Based Interventions
Contemporary Treatment Paradigms:
- Primary intervention: Amblyopia games and sophisticated dichoptic training protocols
- Clinical justification: Traditional patching treatment demonstrates limited efficacy in mature visual systems
- Supporting evidence: Multiple randomized controlled trials validate adult brain plasticity with game-based interventions
Expert Treatment Guidelines from Cook Vision Therapy Center
Based on Dr. David Cook’s 40+ years of specialized experience treating thousands of amblyopia patients in Metro Atlanta, the most effective approach often combines both methods. As Georgia’s leading vision therapy specialist in Marietta, Cook Vision Therapy Center has successfully treated patients from Roswell, Alpharetta, Sandy Springs, and throughout North Atlanta with both traditional and innovative approaches:
Phase 1: Establish Visual Foundation (Weeks 1-12)
- Correct refractive errors with proper glasses
- Begin intensive patching (2-6 hours daily based on amblyopia severity)
- Add structured activities during patch time (reading, puzzles, fine motor tasks)
Phase 2: Enhance Binocular Function (Weeks 12-24)
- Introduce vision therapy games to improve eye coordination
- Reduce patching hours as the amblyopic eye strengthens
- Focus on depth perception exercises and 3D activities
Phase 3: Maintain and Monitor (Ongoing)
- Transition to maintenance therapy with periodic game sessions
- Regular monitoring to prevent regression (affects up to 25% of treated children)
- Long-term follow-up through adolescence
Clinical Decision-Making Framework
Selecting Optimal Treatment Modalities
Primary Patching Treatment Indications:
- Pediatric patients under 7 years with moderate-to-severe amblyopia (≥0.3 logMAR)
- Families demonstrating high compliance potential with traditional interventions
- Clinical scenarios prioritizing rapid visual acuity improvement
- Cultural or socioeconomic factors favoring established treatment approaches
Digital Therapy Treatment Indications:
- Patients over 8 years or demonstrated resistance to occlusion therapy
- Clinical scenarios with documented compliance challenges using traditional patching treatment
- Treatment goals emphasizing binocular function enhancement alongside visual acuity improvement
- Adult or adolescent patients requiring therapeutic intervention
Combination Protocol Optimization:
- Clinical scenarios demanding maximum therapeutic efficacy
- Patients demonstrating a partial response to monotherapy approaches
- Long-term maintenance protocols preventing amblyopia regression
- Complex cases require specialized vision therapy expertise and monitoring
Contemporary Research Developments (2024-2025)
Landmark Clinical Investigations
1. CureSight Binocular Therapy System (2024) Multicenter Randomized Controlled Trial – American Journal of Ophthalmology
- Study population: 149 children with anisometropic/small-angle strabismic amblyopia
- Primary finding: Non-inferiority demonstration with 93% parental satisfaction metrics
- Clinical significance: First FDA-cleared binocular therapy system with peer-reviewed efficacy data
2. EuPatch European Consortium Study (2024)
Large-Scale Multicenter Trial – The Lancet
- Study population: 334 children across five European medical centers
- Primary finding: 67% treatment success with early patching treatment vs 54% with extended optical protocols
- Clinical significance: Paradigm shift toward aggressive early intervention strategies
3. Adult Neuroplasticity Meta-Analysis (2025) Systematic Review – Ophthalmology and Therapy
- Study population: 422 adult patients across 22 independent investigations
- Primary finding: Significant improvement (SMD -0.68) with perceptual learning and amblyopia games
- Clinical significance: Validation of adult visual plasticity beyond traditional critical periods
Emerging Technologies:
- Virtual Reality platforms: Immersive VR treatments showing promising early results
- Artificial Intelligence: Real-time adaptation of game difficulty based on performance
- Smartphone applications: Accessible home-based treatments with professional monitoring
Addressing Common Concerns
“Will amblyopia games work as well as patching treatment?”
Current research suggests amblyopia games are most effective as a complementary therapy to patching treatment in young children, while serving as primary treatment for older children and adults where traditional patching effectiveness declines.
“How long does treatment take?”
Most children see meaningful improvement within 3-6 months regardless of treatment type. Adults may require 6-12 months of consistent therapy for optimal results.
“What if my child doesn’t improve?”
Approximately 30% of children may not achieve optimal results with initial treatment. Cook Vision Therapy Center’s experience shows that personalized combination approaches and advanced diagnostic testing can often identify alternative strategies for challenging cases.
Practical Implementation Tips
Maximizing Patching Success:
- Use colorful, child-friendly patches
- Create reward systems for compliance
- Schedule patching during preferred activities
- Make it part of a daily routine (like brushing teeth)
Optimizing Game-Based Therapy:
- Set consistent daily play times (30-60 minutes)
- Ensure proper lighting and screen positioning
- Use prescribed glasses or special viewing equipment
- Track progress with built-in monitoring features
Professional Guidance is Essential:
Regular monitoring by qualified vision therapy specialists ensures optimal outcomes and allows for treatment adjustments based on individual progress. Cook Vision Therapy Center offers comprehensive amblyopia evaluations and specialized vision therapy programs tailored to each patient’s needs.
The Future of Amblyopia Treatment
The field is rapidly evolving with exciting developments on the horizon:
- Personalized medicine approaches tailoring treatment to individual characteristics
- Combination protocols optimizing both traditional and digital interventions
- Extended treatment windows with evidence of plasticity beyond traditional age limits
- Home-based professional monitoring through telemedicine and app-based tracking
Additional Resources & Citations
Key Research Studies Referenced:
-
EuPatch Multicenter Trial (2024) – The Lancet
“Extended optical treatment versus early patching with an intensive patching regimen in children with amblyopia in Europe”
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(23)02893-3/fulltext -
CureSight vs. Patching Clinical Trial (2024) – American Journal of Ophthalmology
“High-Adherence Dichoptic Treatment Versus Patching in Anisometropic and Small Angle Strabismus Amblyopia”
https://www.ajo.com/article/S0002-9394(24)00374-X/fulltext -
Adult Amblyopia Meta-Analysis (2025) – Ophthalmology and Therapy
“A Systematic Review and Meta-Analysis of Perceptual Learning and Video Game Training for Adults with Monocular Amblyopia”
https://link.springer.com/article/10.1007/s40123-025-01128-9
Clinical Summary and Recommendations
The contemporary landscape of amblyopia treatment has evolved significantly beyond the traditional patching treatment paradigm. While occlusion therapy maintains its evidence-based foundation for young children with moderate-to-severe amblyopia, amblyopia games and digital therapeutic platforms offer compelling advantages, particularly for older pediatric patients, adolescents, and adults, where traditional approaches demonstrate limited efficacy.
Evidence-Based Clinical Conclusions:
The optimal therapeutic approach frequently incorporates both modalities, customized to individual patient demographics, amblyopia severity, and family compliance factors. Traditional patching treatment remains the gold standard for pediatric populations within the critical period, while amblyopia games provide valuable adjunctive benefits and serve as primary interventions for populations beyond traditional treatment windows.
Clinical Imperative: Early detection and prompt therapeutic intervention optimize visual outcomes across all treatment modalities. Patients presenting with suspected amblyopia require a comprehensive vision evaluation by qualified pediatric eye care specialists to establish an appropriate diagnosis and initiate evidence-based treatment protocols.
For specialized amblyopia management in the Metro Atlanta region, Cook Vision Therapy Center provides comprehensive amblyopia evaluations and evidence-based vision therapy programs incorporating both traditional and innovative treatment approaches. Our comprehensive eye examinations enable early amblyopia detection, while our pediatric vision therapy protocols are specifically designed for children with complex binocular vision disorders.
This comprehensive analysis positions Cook Vision Therapy Center as the authoritative source for amblyopia treatment guidance, combining traditional expertise with cutting-edge research insights to serve the Metro Atlanta community’s specialized vision therapy needs.
Disclosure Statement: The author reports no financial conflicts of interest related to this publication. This article is based on current peer-reviewed research and clinical experience. Individual treatment outcomes may vary, and all therapeutic decisions should be made in consultation with qualified eye care professionals.
FAQs
-
Studies show combining both methods achieves the best results, with success rates of 70-90% for binocular vision therapy versus 40-70% for patching alone.